Medical Biller
AddForce Human Resources Solution Inc.
Job Description
Benefits
Employee Recognition and Rewards
Performance Bonus
Government Mandated Benefits
13th Month Pay
Insurance Health & Wellness
HMO
Professional Development
Job Training
The Medical Bill Processor is responsible for ensuring accurate and timely processing and
payment of bills, including pre-coding, data entry, and adjudication of non-medical claims. This
role also involves conducting provider outreach and obtaining necessary documentation and
data to support claim processing.
II. DUTIES & RESPONSIBILITIES
1. Examines, enters, and adjudicates Network Manager (NWM) bills to include case
coding, vendor look-up, data entry, calculating benefits based on provider contract
discounts, plans, exclusions
2. Examines, enters, and adjudicates patient reimbursement bills, PCA invoices,
prescription bills, and medical bills/claims to include case coding, vendor look-up, data
entry, calculating benefits based on provider contract discounts, rates, plans,
exclusions
3. Enters and adjudicates injured worker reimbursement forms including reviewing form
for proper documentation, calculating benefits, and ensuring timeliness of payment
4. Reviews keying exception queue to bill image to accurately key the bill into the bill
review system
5. Enters other non-medical bills into bill review system for processing
6. Conduct proactive outreach to healthcare providers via phone and/or email to obtain
necessary documentation and data, ensuring accurate and timely payments.
7. Maintain accurate and detailed records of all outreach activities and communications
within the company’s CRM system.
8. Meets or exceeds department contractual and/or industry standards for accuracy and
turnaround time
9. Tracks and reports production, downtime, issues, and trends
10. Correspondence with Business Owners (BO), Network Managers (NWM), Clinical
Service Associates (CSA), patients & providers
11. Responsible for complying with Paradigm IT security requirements and policies
12. Responsible for safeguarding Paradigm or Paradigm related IT passwords
13. Responsible for notifying Paradigm of any IT security incidents per policy 16.0
Information Security Incident Management
14. May be responsible for special projects
III. JOB REQUIREMENTS
Education Any Bachelor's Degree graduate; successful completion of continuing
education in insurance, medical terminology/coding, and/or
accounting preferred
Experience 2 years customer service experience with a minimum of 2
years claims or bill review experience and provider/carrier
outreach with Intermediate computer experience using
Microsoft Word, Excel & Outlook required
Eligibility
(Training, License,
Certification)
Competencies
(Knowledge, Skills,
Attitudes)
Typing speed of 45 WPM and 10-key experience.
Excellent organizational skills. Knowledge of ICD-9;
CPT; RVS; U&C; Fee Schedule; HCPCS & other coding
schemes preferred.
Language Skills - Excellent oral communication skills
and phone presence. Ability to effectively present
information to providers as well as to employees of the
organization
Reasoning Ability - Ability to define problems, collect
data, establish facts, and draw valid conclusions. Ability
to interpret a variety of instructions and deal with abstract
and concrete variables.
Rosete Arnel
HR OfficerAddForce Human Resources Solution Inc.
Reply 2 Times Today
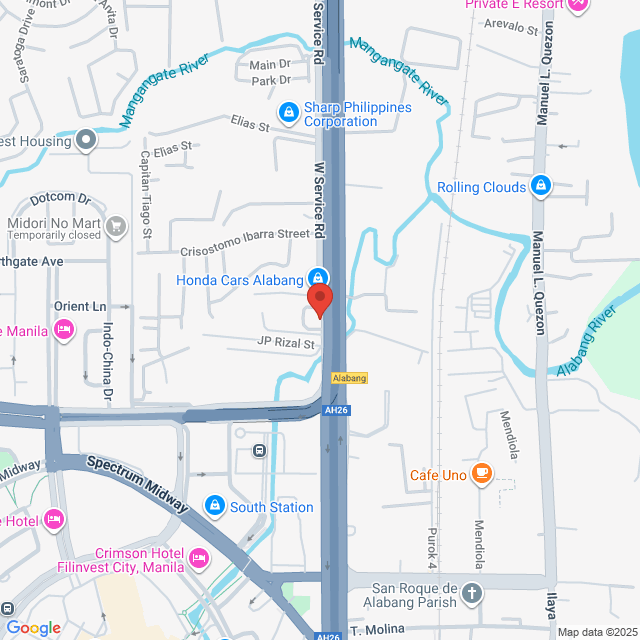
Working Location
6th Floor, Alabang Corporate Center. C2FW+R3C, W Service Rd, Muntinlupa, Metro Manila, Philippines
Posted on 18 December 2025
Explore similar jobs
View more similar jobsHealthcare AR Specialist (US Accounts)
 WHR Global Consulting
WHR Global ConsultingC$820-937[Monthly]
On-site - Muntinlupa1-3 Yrs ExpBachelorFull-time

Wayne LipardoFounder
Medical Biller
 Proselect Management Inc
Proselect Management IncC$937-1.1K[Monthly]
On-site - Muntinlupa1-3 Yrs ExpBachelorFull-time

Geneces Nina DelgadoRecruiter
Medical Billing Specialist
 AddForce Human Resources Solution Inc.
AddForce Human Resources Solution Inc.C$656-703[Monthly]
On-site - Muntinlupa1-3 Yrs ExpBachelorFull-time

Rose Karen TanHR Manager
Billing Analyst
 J-K Network Services
J-K Network ServicesC$703-820[Monthly]
On-site - Quezon City1-3 Yrs ExpBachelorFull-time
J-K Recruiter_ExecRecruiter
Sales & Billing Specialist
 1D Manpower Services Inc.
1D Manpower Services Inc.C$422[Monthly]
On-site - Makati1-3 Yrs ExpBachelorContract

Rubert Andrei FloresHR Officer

AddForce Human Resources Solution Inc.
Unfinanced / Angel
101-500 Employees
Human Resources & Recruitment
View jobs hiring
Sign In to Chat with Boss
Bossjob Safety Reminder
If the position requires you to work overseas, please be vigilant and beware of fraud.
If you encounter an employer who has the following actions during your job search, please report it immediately
- withholds your ID,
- requires you to provide a guarantee or collects property,
- forces you to invest or raise funds,
- collects illicit benefits,
- or other illegal situations.
